Information under Clause 'B.1.11' Of Minimum Standard Requirement Regulations, 1999 and as amended.
Introductions :
Carcinoma of the lungs have continued to baffle clinicians by virtue of their ability to present in myriad ways. We present here the case of a woman who presented with neurological symptoms as a result of cerebral metastases from a lung adenocarcinoma. She was treated as a case of CNS tuberculosis initially but soon came back with new symptoms which raised the suspicion of a malignancy.
Case Description :
History
A 45 year old female initially presented to us with disequilibrium for one month and low grade fever for three months. The patient complained of a tendency of falling to either side while walking in absence any significant weakness of her limbs. There was no history suggestive of any limb in-coordination either. The associated fever was intermittent in nature but was not associated with any headache, neck stiffness, unconsciousness or convulsion.There were no respiratory symptoms like cough, hemoptysis, dyspnea or chest pain. No other localizing features were present either.
Examinations:
Neurological examination was suggestive axial cerebellar disease. There was no neck rigidity and no signs of raised ICT. Respiratory system examination was normal. Other systems were also normal.
Investigations:
Chest skiagram revealed reticulonodular opacities in bilateral middle and lower lung fields (FIGURE 1). Sputum for AFB and Tb-PCR were, however, negative. An MRI Brain revealed multiple ring-enhancing lesions with adjacent cerebral edema in the right frontal, left temporal cortex and left frontoinsular subcortical region (FIGURE 2). She was next sent for an MR spectroscopy which showed lipid peaks in the central part of the lesions whereas the peripheral pat showed mildly elevated choline peak and choline-creatine ratio (FIGURE 3). These features were suggestive of a granulomatous lesion, likely tuberculoma.
Treatment:
The ataxia was thus determined to be due to a lesion involving the cerebellar connections. Treatment was started with antitubercular drugs and steroids.
After one week, however, she came back with a painful swelling of her right leg (FIGURE 4) which was detected to be due to deep venous thrombosis of the right femoral and popliteal veins on colourdoppler. She was also found to have developed superficial thrombophlebitis on her left upper arm (FIGURE 5). A search for occult internal malignancy was made.
She was sent for a whole body PET-CT which revealed a speculated mass in the left lower lobe of lung, the likely primary lesion, along with mediastinal lymphadenopathy and multiple cerebral and skeletal metastases (FIGURE 6). CT-guided FNAC was done from the lung massand the sample was sent for cytopathology. Pathologists confirmed the presence of adenocarcinoma.
Conclusions : Ring enhancing lesions are a common finding on brain imaging and are commonly due to tuberculomas, neurocysticercosis or tumors, both primary and metastatic. MR spectroscopy is usually reliable in differentiating between these diseases but failed to help the diagnosis in this case. Presence of lipid peak plays an important role in identifying tuberculomas[1] and it was on the basis of this specific finding that a probable diagnosis of tuberculoma was made on the MR Spectroscopy report. Trousseau’s syndrome of recurrent or migratory thrombophlebitis is a marker of occult malignancy and should not be missed in any individual.
Discussion :
Multiple ring-enhancing lesions of the brain are one of the most commonly encountered abnormalities on neuroimaging. They can be caused by a variety of infectious, neoplastic, inflammatory or vascular diseases. Distinguishing non-neoplastic causes from neoplastic lesions is extremely important because a misdiagnosis can lead to wrong administration of ATD and delaying diagnosis of malignancy. Meticulous clinical evaluation and relevant investigations are required for making a definitive diagnosis. Newer advanced diagnostic techniques, such as diffusion-weighted magnetic resonance imaging (MRI), perfusion-weighted MRI, magnetic resonance spectroscopy, single-photon emission tomography and positron emission tomography may help in establishing the etiology. However, early brain biopsy is often needed because several of these diseases are potentially life-threatening. But PET CT whole body in selected cases can diagnose malignancy without reverting to brain biopsy.
Primary and metastatic tumors, on imaging, manifest as rounded, well-circumscribed, ringenhancing lesions of variable sizes surrounded by a variable amount of perifocal vasogenic edema.
Metastatic lesions are typically subcortical, occurring in or near the gray matter-white matter junction, and are usually associated with severe perilesional edema. MRI typically reveals mild T1 hypointensity with T2 hyperintensity and fluid-attenuated inversion recovery hyperintensity at the site of the lesion. After contrast administration, a nodular ring pattern of enhancement is seen. Metastases from malignant melanoma may demonstrate T1 hyperintensity because of hemorrhagic or melanin components of the lesion[2].
Tuberculomas are frequently encountered brain lesions in tropical countries. Tuberculoma usually appears hyperintense on T2-weighted and slightly hypointense on T1-weighted images. Tuberculomas on contrast administration appear as nodular or ring-like enhancing lesions[3].
MRS shows a lipid peak in and it plays an important role in identification of tuberculomas from other infective granulomas[4]. Lactate peak may also be seen. In a study published in 2011, higher ratios of Cho/NAA and Cho/MI accompanied by lower ratio of NAA/Cr were associated with the most probability for malignancy. Lactate and lipid peaks have been also observed in malignant tumors[5].
Rahul Awasthi et al presented a case of primigravida at 30 weeks of pregnancy diagnosed as metastatic adenocarcinoma cerebrum, which radiologically mimics intracranial tuberculoma with its primary focus on originating from the lungs[6].
CT/MRI of the brain is the usual initial investigation done when a intracranial mass is suspected. However, the diagnosis may be complicated by ambiguous radiologic findings; thus the tissue biopsy remains the gold standard[7].

Figure : 1 Chest x ray showing reticulonodular opacities
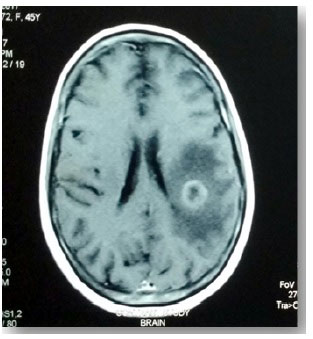
Figure : 2 MRI Brain showing ring enhancing lesion

Figure : 3 MR Spectroscopy Brain showing lipid peak

Image 4 : Showing infiltration of drug in QL BLOCK

Figure : 3 MR Spectroscopy Brain showing lipid peak

Figure : 6 PET-CT Thorax showing speculated left lung nodule

Figure : 7 FNAC Slide of tissue from lung mass showing adenocarcinoma
1. Jayasundar R, Singh V, Raghunathan P, Jain K, Banerji A. Inflammatory granulomas: evaluation with proton MRS. NMR in Biomedicine. 1999; 12(3):139-44.
2. Young RJ, Sills AK, Brem S, Knopp EA. Neuroimaging of Metastatic Brain Disease. Neurosurgery 2005;57:S4- 10-S4-23.
3. Smirniotopoulos JG, Murphy FM, Rushing EJ, Rees JH, Schroeder JW. Patterns of contrast enhancement in the brain and meninges. Radiographics 2007; 27:525- 51.
4. Jayasundar R, Singh V, Raghunathan P, Jain K, Banerji A. Inflammatory granulomas: evaluation with proton MRS. NMR in Biomedicine. 1999; 12(3):139-44.
5. Aydin H, Sipahioðlu S, Oktay NA, et al. The value of proton MR-spectroscopy in the differentiation of brain tumours from nonneoplastic brain lesions. 2011; 94:1- 10.
6. Rahul Awasthi, Nilesh Jain, Shrikant Rege, RaghwanIyengar, Abhishek Songara. Metastatic Adenocarcinoma Cerebrum Mimicking Tuberculoma in Pregnancy : A Case Report with Review of literature. Department of Neurosurgery, Sri Aurobindo Medical College and PG Institute, Indore, Madhya Pradesh, India.
7. Saini KS, Patel AL, Shaikh WA, Magar LN, Pungaonkar SA. Magnetic resonance spectroscopy in pituitary tuberculoma. Singapore Med J 2007; 48 (08) 783-786.
Ramakrishna Mission Seva Pratishthan Vivekananda Institute of Medical Sciences
99, Sarat Bose Road
Kolkata – 700 026
Phone: +91 33 2475 3636-3639
Fax: +91 33 2475 4351
Emails: rkmspsmvims@gmail.com
Copyright 2019, Ramakrishna Mission Seva Pratishthan, All Rights Reserved
Design and Development by Inforace Solutions Pvt. Ltd.